Instaskills, n,
one paged quick learning so you can hit the ground running while on the job
Commissioning Public Health Services
Public health work can be divided into health services we provide (e.g. health promotion and health improvement like healthy eating at schools, smoking cessation, community services for older people etc) and health services we commission (e.g. immunisation programmes, screening programmes, school nursing services, care pathways for obesity etc). Good commissioning of services is a cornerstone of universal healthcare; the others being health technology assessments, strong provision and access to primary health care and good human resources/workforce for health.
Most commissioning revolves around block contracts or 'payment by results' contracts between commissioners (NHS England/Improvement, Clinical Commissioning Groups and local authorities) and providers such as acute trusts (i.e. hospitals), ambulance trusts, mental health trusts and the independent sector. There are also contracts with the voluntary or third sector. NHS commissioning is focused on developing care standards, quality improvement of provider services and value for (tax)payer's money.
Previous to April 2013, public health teams largely contributed to commissioning in terms of helping to establish needs and priorities (at the start of the commissioning cycle) and with the evaluation at the end of the cycle. Often, public health teams were involved in monitoring KPIS in contracts with community providers or acute services providers. However, since April 2013, many public health teams are part of commissioning teams or are commissioners of services. Much of this commissioning work involves contract management, budget lines and invoicing and performance monitoring and management.
Commissioning is the buying, weighing up of cost-effective ways of delivering something and inspiring someone to look after health and well-being differently. In our personal lives, we have all been involved in commissioning - e.g. when going on holidays, we may go on a website and weigh the different holidays available for our budget and which one offers the best value for our limited funds. All commissioning in NHS is covered by the 2009 Procurement Regulations and encompasses the ideals of corperation and competition - i.e. best value for money, testing the market and getting the best cost-effective service to fit the market. The Corperation and Competition Panel regulates commissioning in England.
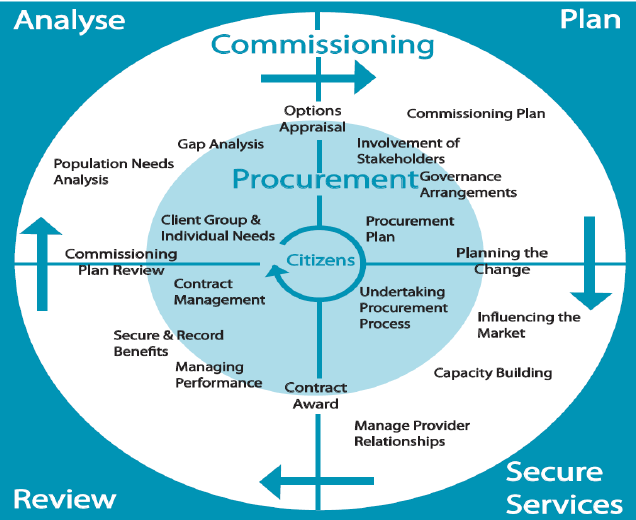
Stages in Commissioning
1. Assessment and Planning
2. Procurement and Contracting
3. Performance Management, Settlement and Review
4. Patient and Public Engagement
Throughout the commissioning cycle, public health skills are needed in the planning (needs assessment, review of evidence, deciding priorities), designing and procuring services of a high quality standard and finally, by managing performance, monitoring quality and evaluating service provision.
To commission services, you will need to know:
- Needs of the population
- What services are available?
- What changes are needed?
- Agree how and where to purchase.
- Monitor performance of providers against agreed contracts.
How do you decide what to commission?
Health authorities setting up contracts with hospitals will need to decide between different services and which should have priority. In Health of Nation, Department of Health set up the principles for the development of services (1) effectiveness (2) efficiency and (3) health improvement. You will need to decide between values of high quality or cheapness or compromise.
To commission any service, you need the element of a perfect market (i.e. many buyers and sellers, free entry and exit, homogeneous product, perfect information and no externality (i.e. I pay and someone else benefits).
For specialist commissioning (this is for rare conditions e.g. for haemophilia or chronic kidney disease, specialised cancer services, motor neurone disease etc), you will also need to consider insurance, high costs, whether or not population demand is predictable and whether an individual's probability of demand is independent.
Commissioning services is based upon Bradshaw's 'Need, Supply and Demand' model. Balancing demands and need requires a set of values upon which health services provision can be based.
These values are:
- Equity (expensive treatments are limited in favour of the cheaper)
- Greatest potential for improving health (purchasing is based on the greatest number of lives saved and disabilities avoided e.g. smoking prevention by the GPs tends to be the most effective here)
- Accessibility (this tends to favour primary care; acutely ill people have less priority)
- Best possible service for everyone (these services are likely to run out of money because of spending on services of marginal value)
There are a number of factors that influence the quantity of services needed. These are disease incidence and prevalence including 'new' diseases (Incidences and prevalence measures do not automatically provide a measure of 'need' for health care); Medical technology and other pressures such as public opinion, politicians, press, voluntary groups and community health councils.
Commissioning in Practice
1. Commissioning starts looking at feedback, audits, needs assessments, national service specifications, NICE guidance etc to inform this year's commissioning strategy and intentions. This can involve putting together a business case using activity out-turn, cost card and population growth. This may include noting cost pressures.
2. If there are to be changes to the contract - this will be a variation to contract and will require 30-90 days notice. All NHS contracts usually last 3 years but can be extended 12-24 months. Alteration to service specification will need agreement by both parties (commissioner and provider). Directed Enhanced Services and National Enhanced Services run for 3 years and don't need signing each year.
3. Sometimes you need to decommission a service and this will require 90 days notice except when in the first 24 months of a contract, where 12 months notice is needed. The notice letter to the provider comes from the CEO. Once decommissioned, there will need to be a closure plan with provider and clients. If the service is to be recommissioned, a procurement strategy and plan is needed (this is the same for the commissioning of a new service). Any contract that is over £173,000 per annum must have competition in tendering but Legally, you don't have to procure for amounts under £173,000. Single Tender Action can be cited. Single tender action restricts procurement to any qualified provider that can deliver this service. Used if small monies and short timeframes. You can skip PQQ1 and PQQ2 stages of the pre-qualification questionnaire. Since 2010, tendering uses delta portal which outlines all expressions of interest, pre-qualification questionnaire and invitations to tender. Every tender over £300,000 appears on Delta Portal. Procurement can take 90 days.
4. Performance Management - if KPIs are not met, you ask for an action plan within 30 days. If this plan fails, then you opt for remediation (i.e. tell them to do something by a certain time) and if that fails, it is a breach of contract. You serve a breach (usually means taking money off them).
Commissioning in a Financial Uncertainty
This involves looking at a service(s) and deciding how you can best deliver this service (i.e. maintain and improve quality) within a budget. It very often leads to more efficient and effective services. Procedures used include:
1. Decommission unnecessary or ineffective interventions
2. Use methodologies for taking costs out of the system
3. Redesign services
4. Move services, where appropriate, from acute trust to community
5. Collaborative procurement between partners
As a public health commissioner this is about balancing what should be (clinical gold standards), what is value for money (commissioner organisation viewpoint) and what is the best you can do with the resources you have ('good enough for the tax-payer). Cost-effectiveness and cost benefit analyses are useful tools to have.
Payment by Results
This has been in operation since 2003. Prior to that, block contracts were awarded to acute trusts (and mental health trusts) to provide services with prices based on historic local costs and negotiating skills. It was difficult for commissioners to see what outputs actually cost and to identify and deal with inefficiency by the provider. With payment by results (or really it is payment by activity), there is a set tariff per activity and income is generated by the provider by simply multiplying the price by activity. Pricing is determined through classification (i.e. a system of codes is used to record clinical diagnosis and procedures in a standardised way), currency (i.e. codes are grouped together on the basis of clinical and financial similarity to provide standardised units for payment knowns as health resource groups) and costing (i.e. there is a standard price allocated to the health resource groups on the basis of the reported cost of provision across the acute sector).
Payment by results has helped to strengthen commissioning. You can monitor provider activity and performance and can now focus on demand management.
Demand Management
This was first raised in the NHS Operating Framework (2006/7) and was used as part of practice based commissioning which then became CCG commissioning. Under the NHS Operating Framework, demand management was said to consist of three components. Firstly, practice based commissioning was said to be an effective demand management measure as it ensured that all GP practices have the incentive to control referrals and other use of services. This freed up resources which could be re-invested to improve services. Secondly, commissioners could have provisions in contracts with hospitals, for instance, having expected clearance times for existing waiting lists, to help demand management and finally, there should be monitoring arrangements. CCGs and acute trusts should have joint responsibility for agreeing measures to deal with significant variance from plan, for example, freeing up resources for redeployment when activity is reflecting changes in patient choice or if there is a genuine unexpected increase in demand for a service.
Demand management has focused on hospitals who are operating high levels of activity and comprises of redesigning pathways and referral management. To have appropriate effective efficient health services for patients, you need:
- effective management of elective referrals
- alternative primary care provision using GPs with special interests;
- A&E diversion schemes back to primary care
- effective contractual arrangements.
Public health have been involved in some places in reviewing the referral process and pathways (including appropriateness of GP referrals and making consultant-to-consultant referall pathway more effective), reviewing treatment times, helping to develop primary care provision points instead of A&E where possible and helping to develop effective case management by communicating and installing best practice guidance.
QIPP & CQUIN
In 2011, QIPP was developed as part of world class commissioning processes under the then Labour Government. The idea was to give PCTs the skills to be at the forefront of delivery improvements to all parts of their local population using principles of QIPP (Quality, Innovation, Productivity and Prevention). World Class Commissioning may have ceased but QIPP continues to be used today with all NHS organisations - providers included - devising annual QIPP plans to demonstrate efficiency and value for money.
CQUIN stands for Commissioning for Quality and Innovation. Under a CQUIN, you can earn up to 2.5% of contract value - usually 12months long. It is used to upscale and uplift a service above and beyond service delivery.
Useful Glossary
|
Term |
Description |
|
|
|
|
Bidder |
A single operating organisation/person that has been short-listed through the PQQ evaluation process and been invited to participate in the ITT stage and is bidding for one or more Schemes |
|
Bidder Guarantor |
An organisation providing a guarantee, indemnity or other undertaking in respect of a Bidder’s or a Bidder Member’s obligations |
|
Bidder Member |
A shareholder or member or proposed shareholder or member in, or controlling entity of, the Bidder and / or that shareholder’s or member’s or proposed shareholder’s or member’s ultimate holding company or controlling entity |
|
CPD |
Continuing Professional Development |
|
Clinical Services Supplier |
All suppliers providing clinical services which are the subject of the Contract including, but not limited to, general dental services |
|
Contract |
The National Standard Contract for Goods and Services |
|
DH |
Department of Health |
|
EOI |
Expression of Interest |
|
FOIA / Freedom of Information Act |
The Freedom of Information Act 2000 and any subordinate legislation made under that Act from time to time, together with any guidance and / or codes of practice issued by the Information Commissioner, the Department of Constitutional Affairs, the Office of Government Commerce and the NHS in relation to such legislation or relevant codes of practice to which the DH and NHS England (London) is subject |
|
GAD |
Government Actuary’s Department |
|
IM&T |
Information Management and Technology |
|
ITT |
Invitation to Tender |
|
MOI |
This Memorandum of Information setting out the details of each NHS England Scheme and the requirements of the NHS England (London) Procurement |
|
NHS |
National Health Service |
|
NHS England |
The Commissioner |
|
Lot |
A defined service area which makes up one geographical service area within London. |
|
Potential Bidder |
A single operating organisation or person that is participating in the NHS England (London) Procurement, but that has not at the relevant time been invited to respond to an ITT |
|
PQQ |
Pre-Qualification Questionnaire |
|
Provider |
The successful Bidder who has entered into a Contract with The commissioner to provide the Administration Hub and Clinical service or Clinical Service(s) |
|
Relevant Organisation |
An organisation(s) or person connected with a response to a PQQ and / or connected with a bid submission including (without limitation): (i)the potential Bidder; (ii)the Bidder; (iii)the Provider; (iv)each Bidder Member; (v)each Bidder Guarantor; and (vi)each Clinical Services Supplier |
|
Scheme ITT |
An ITT that is specific to those services set out in one or more NHS England Schemes that the Commissioner wishes to procure and is sent to potential Bidders who have been short-listed following the PQQ stage |
|
TUPE |
Transfer of Undertakings (Protection of Employment) Regulations 2006 (SI/2006/246) |
|
VfM |
Value for Money which is the optimum combination of whole-life cost and quality (fitness for purpose) to meet the overall service requirement |